How are brain aneurysms treated?
Outlines the main treatment approaches for brain aneurysms, comparing coiling, clipping, and newer devices, and explains how doctors decide which option is best.
What are the main treatment paths?
Treatment aims to secure the aneurysm and prevent bleeding or rebleeding. Options include endovascular procedures inside the vessel, or open surgery. Decisions depend on aneurysm features and your overall health, and are best made by a multidisciplinary team.
What is endovascular coiling?
A thin tube is guided into the aneurysm and soft platinum coils are packed inside to block blood flow and encourage healing of the vessel wall. The majority of aneurysms are now treated endovascularly due to the reduced invasiveness.
What is neurosurgical clipping?
A surgeon opens the skull and places a tiny clip across the neck of the aneurysm to stop blood entering it.
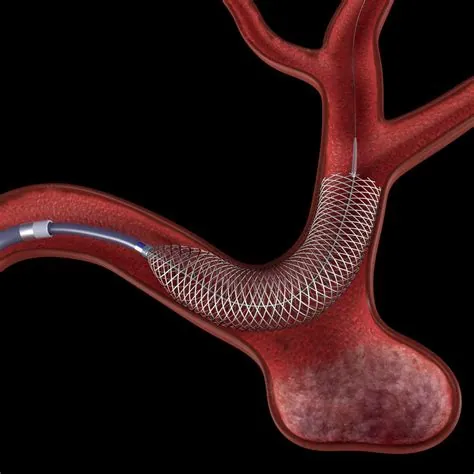
What newer devices might be used?
Specialist centres may use stents to support coils in wide-necked aneurysms, flow-diverting stents to redirect blood along the artery, or intrasaccular devices placed directly in the aneurysm sac. In the acute phase after a bleed, stent-assisted coiling and flow diversion need dual antiplatelet medicines and carry higher risk, so they are reserved for select situations.
How do doctors decide the best approach?
For a ruptured aneurysm, national guidance advises an interventional neuroradiologist and a neurosurgeon to agree a plan with you, choosing between coiling, clipping, or careful monitoring if neither is appropriate. If there has been a bleed, securing the aneurysm should happen as early as possible, ideally within 24 hours, to reduce the risk of rebleeding.
What does the evidence say about outcomes after a bleed?
In the ISAT trial, patients suitable for either treatment had lower death and dependency at one year with coiling than with clipping. Advantages for coiling persisted at 10 and 18 years.
How are unruptured aneurysms managed?
Most do not rupture and can often be monitored. Choices depend on aneurysm size, site and shape, your age and health, and whether the aneurysm is growing. Teams often use tools such as PHASES and ELAPSS to support decision-making, and may recommend monitoring rather than treatment in many cases. Monitoring typically includes strict control of vascular risk factors and interval imaging at 6–12 months, then yearly or every two years, tailored to growth risk.
Key takeaways
- The majority of aneurysms are now treated endovascularly.
- After a bleed, early treatment reduces rebleeding risk.
- Newer options include stents, flow diverters and intrasaccular devices, used selectively.
- Many unruptured aneurysms are monitored rather than treated, using structured risk tools and planned imaging.
Full guide to brain aneurysms
Take control of your health with clear, expert information:
- What brain aneurysms are
- Diagnosis and treatment explained
- When to seek help
Aneurysm