Are there any new treatments for brain aneurysms?
What has changed in brain aneurysm treatment, and what the newest minimally invasive options mean for patients.

Surgical clipping
Surgeons performed clipping, placing a small metal clip across the aneurysm’s neck to seal it. Open surgical clipping of intracranial aneurysms was pioneered in the early twentieth century, with Walter Dandy performing the first successful neck-clipping in 1937. Early procedures carried high risks because of poor visualisation, limited clip designs and inadequate anaesthesia. The introduction of the operating microscope in the late 1950s allowed surgeons to work with far greater precision, while the development of refined craniotomy approaches and more sophisticated clip designs reduced complications and improved vessel preservation. Advances in angiography, CT and MR imaging, along with intraoperative fluorescence techniques, further enhanced accuracy and safety. Modern anaesthesia and intensive care support also played a crucial role in lowering mortality. Over the decades, these innovations transformed clipping from a hazardous operation into a reliable and effective treatment, though its role has more recently been shared with less invasive endovascular methods.
Endovascular treatment
Endovascular treatment works from inside the blood vessels, usually by passing a thin tube from the wrist or groin up to the brain. The first breakthrough came in 1990 with Guglielmi detachable coils, which allowed aneurysms to be packed internally. In 1997, Jacques Moret introduced balloon remodelling, and the same year saw the first stent-assisted coiling, opening the door to treating wider-necked aneurysms. The pivotal ISAT trial in 2002 showed that for ruptured aneurysms suitable for either approach, coiling gave better long-term outcomes than clipping.
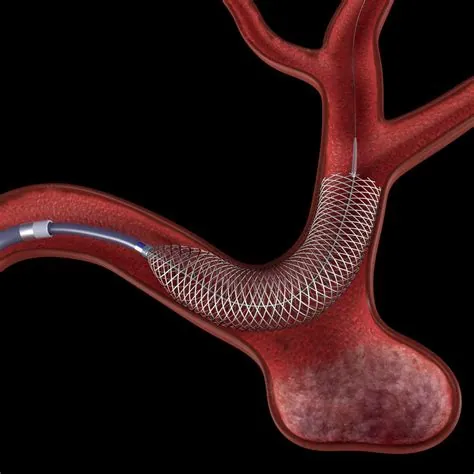
Flow diverters
In 2007, the arrival of flow-diverter stents transformed practice, offering durable reconstruction for large, giant, wide-necked, fusiform or recurrent aneurysms. Flow diverters are fine-mesh tubes placed across the aneurysm neck inside the parent artery, reducing inflow, encouraging clotting within the sac, and promoting vessel healing.
Intrasaccular devices
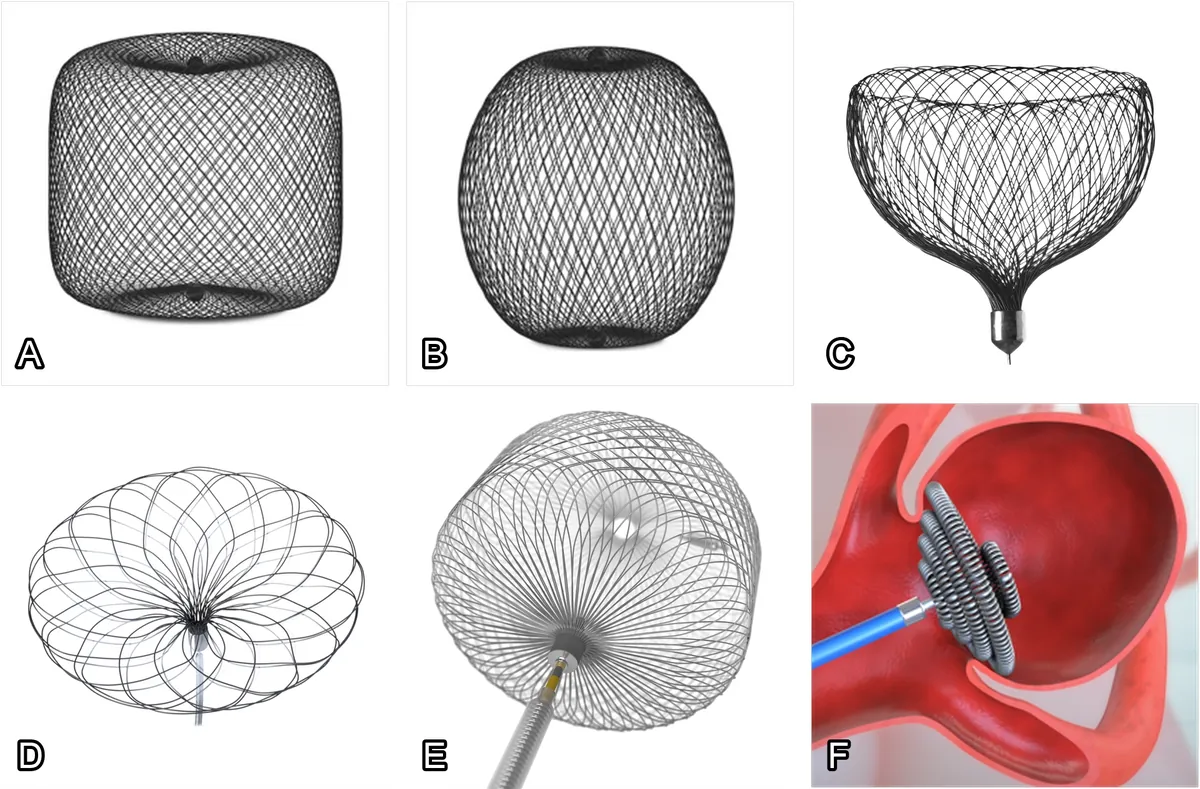
The most recent development are intrasaccular devices. These sit inside the aneurysm itself at the neck, blocking blood entry without the need for a permanent stent. This makes them attractive in bifurcation aneurysms, since long-term dual antiplatelet therapy can usually be avoided.
Intrasaccular devices sit inside the aneurysm itself, typically at the neck, to block inflow. Many of these do not require a permanent stent, so long-term dual antiplatelet therapy is often unnecessary. They are especially attractive for bifurcation aneurysms where two vessels branch at the aneurysm neck. Some evidence suggests intrasaccular devices are the safest way to treat cerebral aneurysms.
- WEB (Woven EndoBridge, MicroVention). The first widely used option, introduced in 2011. It is a soft braided mesh that fills the aneurysm neck. WEB often avoids stents and long-term dual antiplatelets.
- Contour and Neqstent (Stryker). Neck-bridging intrasaccular implants designed to plug the neck. Contour can be used alone in select cases, while Neqstent is intended to be combined with coils passed through its struts to complete occlusion.
- Artisse (Medtronic). A softer device than WEB when constrained, which can make deployment easier in shallow or angled aneurysms. Like WEB, it usually avoids long-term dual antiplatelets.
- Nautilus (EndoStream). One of the most recent devices. It provides neck coverage and a flow-disruption effect, then allows coiling through a central opening. Early series report high occlusion with minimal complications. It is not widely available yet.
What does this progress mean for patients?
Modern treatments now enable a broader range of aneurysm shapes and locations, with shorter recovery, lower complication rates in many scenarios, and durable results. Intrasaccular devices, in particular, reduce the need for permanent stents and strong antiplatelet medication, which is an advantage in both elective and ruptured cases when anatomy allows.
Key takeaways
- Modern care offers more options: coiling, balloon-assisted coiling, stent-assisted coiling, flow diverters, and intrasaccular devices.
- Flow diverters give durable occlusion for large, wide-necked and complex aneurysms.
- Intrasaccular devices like WEB, Artisse, Contour/Neqstent, and Nautilus often avoid stents and long-term dual antiplatelets, while achieving high occlusion rates.
- Since ISAT, many ruptured aneurysms suitable for either approach are treated endovascularly, with better long-term outcomes than clipping.
- Overall, endovascular therapy is becoming safer and more durable, with shorter recovery for many patients.
Full guide to brain aneurysms
Take control of your health with clear, expert information:
- What brain aneurysms are
- Diagnosis and treatment explained
- When to seek help
Aneurysm