Endovascular treatment of aneurysms
Minimally invasive procedures including coiling, stent-assisted coiling, flow diversion, and intrasaccular devices.
The development of endovascular techniques has completely revolutionised the treatment of brain aneurysms increasing the safety of the procedure and reducing the invasiveness and recovery time. The majority of brain aneurysms are now treated using endovascular techniques. There are very few aneurysms that cannot now be treated endovascularly.
What does endovascular treatment involve?
Rather than requiring a large incision and direct surgical access to the aneurysm, endovascular treatment achieves its goal by guiding small, specialized devices through the patient’s blood vessels (the body’s own natural highways) to the site of the aneurysm. Embolisation means to promote clot formation within the aneurysm, commonly by inserting devices such as coils into the aneurysm or placing stents acoss its neck.
How does it work?
All endovascular treatments aim to initiate the body’s natural healing process and involve first filling the aneurysm with a stable clot. This seals off the aneurysm, preventing blood from entering it. The wall of the blood vessel remodels over time, completing the healing and eliminating the aneurysm.
What are the types of endovascular treatment?
- Coiling (Endovascular Coiling or Coil Embolization). This involves small, soft platinum coils being threaded through a catheter and placed directly into the aneurysm.
- Stent-Assisted Coiling. Stents are small, tube-shaped devices that are used in conjunction with coils to provide support to the weakened arterial wall. They also help keep the coils within the aneurysm sac. The stent remains in the artery permanently.
- Flow Diversion. This treatment employs a device called a flow diverter, similar to a stent but with denser walls. It’s placed in the artery carrying blood to the aneurysm. Instead of filling the aneurysm with coils, the flow diverter redirects blood flow away from the aneurysm. This reduced blood flow into the aneurysm promotes clotting within the aneurysm, leading to its closure. Coils are not mandatory but are sometimes also placed.
- Intrasaccular devices such as the Woven Endobridge (WEB). These are placed directly into the aneurysm sac via a catheter, similar to coiling, but are able to treat aneurysms that would otherwise require stents.
How is coil embolisation performed?
Coil embolisation is undertaken during general anaesthesia. The doctor makes a small incision of about 3 mm, typically in the wrist or groin, to access a blood vessel. Following this, they insert a long, thin tube, called a catheter, through the incision into the blood vessel. Using a method called fluoroscopy, which involves real-time X-ray imaging, the doctor is able to navigate the catheter through the patient’s vascular system until it reaches the blood vessels of the brain where the aneurysm is located.
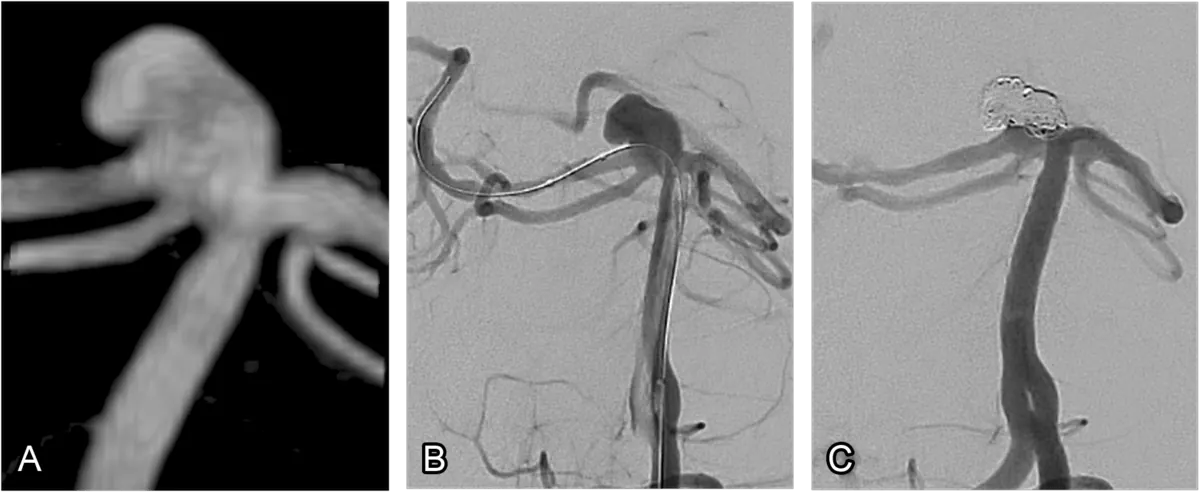
Once the catheter is in position, small platinum coils are threaded through the catheter and into the aneurysm (fig. 1 and fig. 2). These coils are soft and flexible, allowing them to adapt to the shape of the aneurysm. As the blood comes into contact with the coils, it begins to clot, gradually filling up the aneurysm over time. This process effectively isolates the aneurysm from the rest of the circulatory system, thus preventing it from rupturing. The coils are left in place and do not need to be removed.
After the coils are properly placed, the catheter is carefully withdrawn from the body. The patient is usually required to stay in the hospital for the night following the procedure to enable the medical team to monitor the recovery.
What is stent assisted coiling?
Stent-assisted coiling involves the insertion of a small, mesh-like tube called a stent in addition to coils.
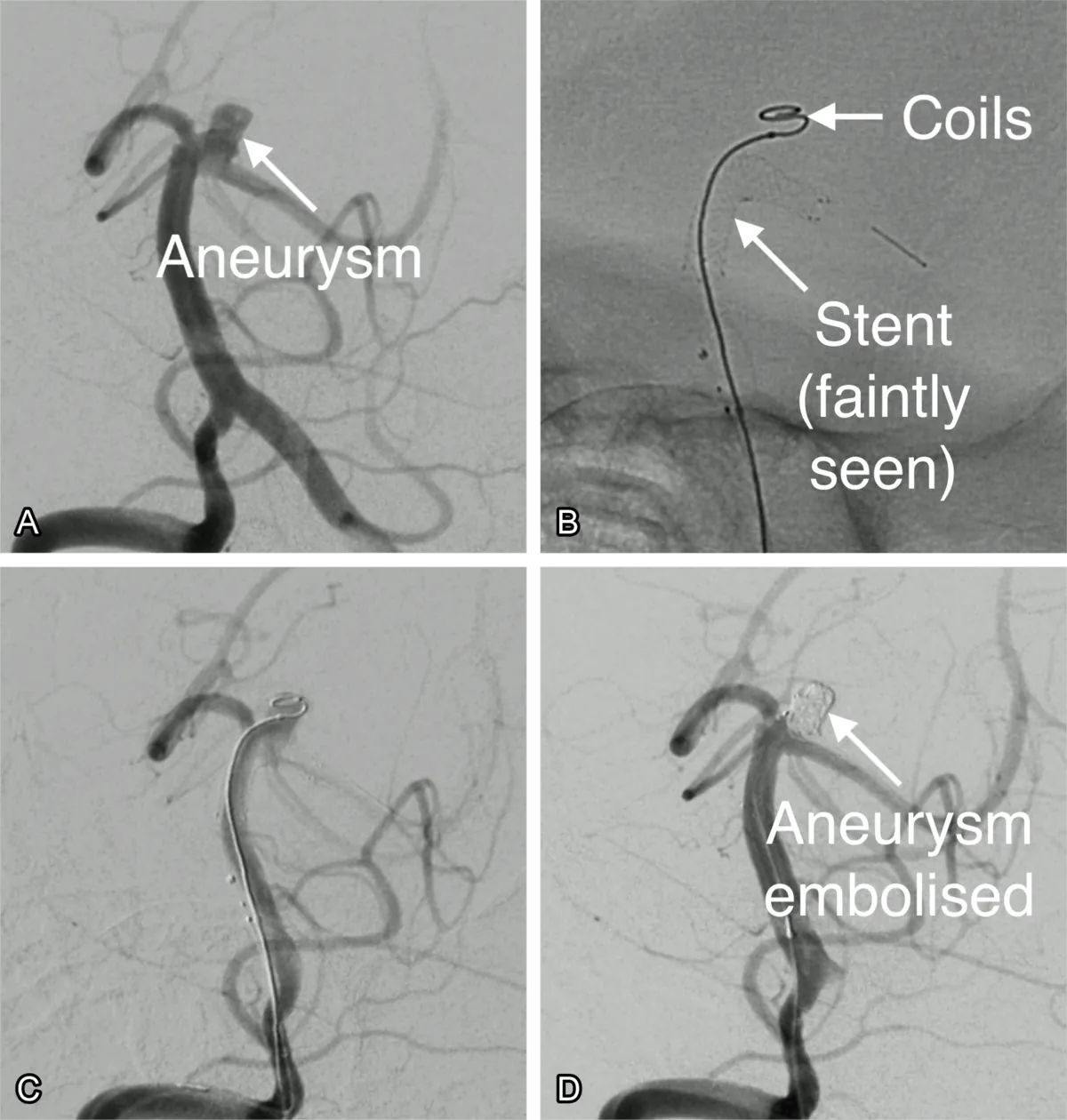
Similar to coil embolisation, a tiny catheter is navigated through the blood vessels, starting from an access point typically in the wrist or groin, all the way up to the site of the aneurysm in the brain. The stent is then placed across the opening of the aneurysm, acting like a small scaffold that provides support to the blood vessel wall, which can be weakened due to the aneurysm (fig. 3 and fig. 4).
Once the stent is in place, small coils are threaded through the catheter and placed into the aneurysm. The coils promote blood clotting, thereby filling the aneurysm and preventing it from rupturing. The stent helps to hold these coils in place and prevents them from slipping into the normal blood vessel. It’s particularly useful in treating wide-neck aneurysms, where the risk of coils slipping into the parent vessel (the blood vessel supplying the aneurysm) is higher. The stent also typically increases the durability of the procedure, reducing the risk of recurrence.
After the procedure, you will likely need to take a course of antiplatelet medications such as clopidogrel, in addition to aspirin. These help to prevent the formation of blood clots around the stent. This is a routine precaution and an important part of ensuring the success of the procedure. Antiplatelet medications are given in low doses and make the platelets in your blood less sticky, reducing the chance that a clot will form. These are often stopped at 6 months, with aspirin continuing for 1-2 years.
What is flow diversion?
Flow diversion is another minimally invasive endovascular treatment designed to manage brain aneurysms. The primary aim of this treatment is to divert blood flow away from the aneurysm and therefore prevent rupture.
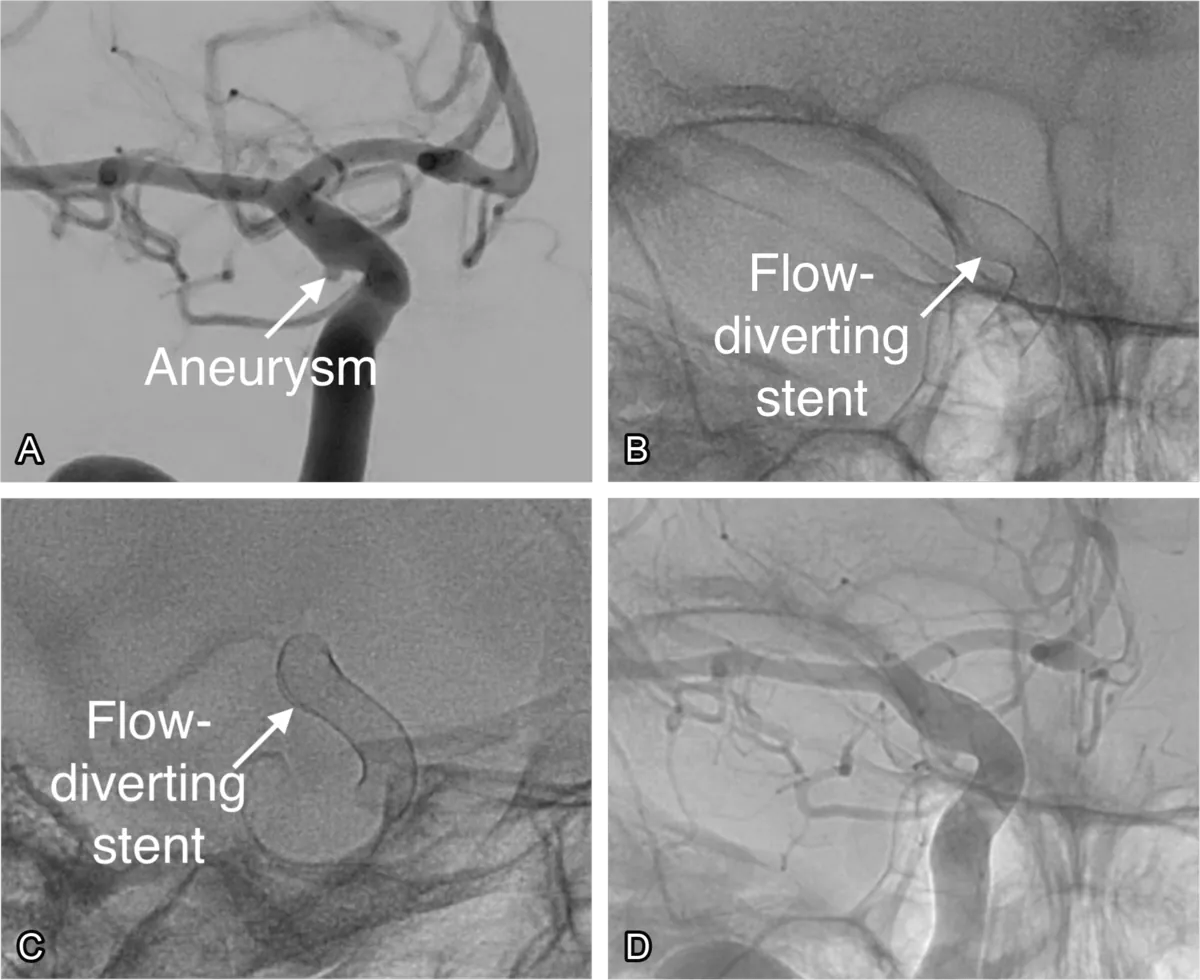
A flow diverter, similar to a stent, is a small tubular mesh device that’s placed inside the parent artery, the blood vessel supplying the aneurysm (fig. 5 and fig. 6). The flow diverter is designed to alter the blood flow dynamics in the artery, thereby diverting blood away from the aneurysm. They can be used with or without placement of coils in the aneurysm.
Over time, this decreased blood flow into the aneurysm encourages the formation of a blood clot within the aneurysm, which helps to seal it off from the rest of the blood vessel. As the aneurysm shrinks and heals, the artery regains a more normal shape and function. This process can take several weeks to months.
Flow diversion is particularly effective for recurrent, large, wide-necked, or thrombosed aneurysms that can’t be adequately treated with other methods. It is also necessary to take a course of antiplatelet medications after insertion of flow diverters.
What is an intrasaccular device?
Intrasaccular devices such as the WEB (Woven EndoBridge) device may be used in the treatment of wide neck aneurysms which would otherwise require stents or flow diverters (fig. 7).
The WEB device, made of ultra-fine braided wires, is a flexible, self-expanding mesh that resembles a tiny basket. It is introduced into the aneurysm using a catheter navigated through the blood vessels from a small incision usually made in the wrist or groin. Once inside the aneurysm, the WEB device expands to fit the shape and size of the aneurysm, serving as a barrier that disrupts the blood flow within. This promotes clot formation within the aneurysm, sealing it off and isolating it from the rest of the circulation, thereby reducing or eliminating the risk of rupture.
A benefit of the WEB device is related to post-procedure medications. With stents or flow diverters, patients are typically required to take antiplatelet medications for a period of time to prevent blood clot formation around the treatment site. However, because of the way the WEB sits in the aneurysm itself rather than the blood vessel, patients usually do not need to take these medications.
Is endovascular treatment durable?
Endovascular treatment is highly effective at permanently eliminating the aneurysm and providing lifelong protection from rupture. For this reason it is now the most common method to treat brain aneurysms worldwide and has been employed to save countless lives.
In preventing adverse consequences such as disability or death endovascular treatment is comparable surgical clipping. It is the recommended treatment in ruptured aneurysms as studies have shown that endovascular treatment is safer.
Recurrences are rare. In a large study at least one further treatment was necessary in 4.9% of patients. They are picked up on follow-up scans and further endovascular treatment can be performed to safely eliminate them. It is important to be aware that recurrences are also possible when the aneurysm is surgically clipped.
The key benefit arises from the low invasiveness of the procedure, reducing harm incurred during the treatment itself.
What are the risks of endovascular treatment?
Endovascular embolisation of aneurysms is normally performed successfully without complication, but all medical treatments carry the potential for risk.
Recovery is usually relatively rapid after endovascular treatment. Patients typically spend one night in hospital for monitoring and are discharged the day after. The site of arterial entry in the wrist or groin might be sore for a few days when it heals. Rarely there are minor side effects like oozing or bleeding from these sites. Applying pressure usually stops this. A small, typically temporary bruise may also form. Occasionally the patient might experience headaches that typically settle over days to weeks.
Serious but rare risks include a 5% chance of stroke from the procedure due to aneurysm rupture or blood vessel occlusion, causing potential limb weakness, speech or vision difficulty which could be temporary or permanent. A very rare 1% risk of a severe brain injury leading to death exists. There is a small chance of vessel damage in the groin or wrist from the catheter entry necessitating surgery.
Aneurysm Brain aneurysm Cerebral aneurysm