Carotid artery stenosis
What carotid artery stenosis is, its risk factors, diagnosis, and treatment options including stenting and endarterectomy.
What is carotid artery stenosis?
Carotid artery stenosis is a narrowing of one or both of the carotid arteries. These large arteries, found on each side of the neck, supply blood to the brain, face and head. Narrowing usually happens because of atherosclerosis, where fatty deposits (plaques) build up inside the artery wall.
When healthy, arteries are smooth and open, allowing blood to flow freely. With stenosis, the passage narrows, making blood flow less efficient. The main danger comes when plaque or a blood clot breaks away and travels into the brain, blocking smaller arteries. This can cause a stroke or, if the blockage is temporary, a transient ischaemic attack (TIA).
How common is carotid stenosis and why does it matter?
Carotid artery stenosis becomes more common with age. It is estimated that up to 5% of the general population may have some degree of narrowing. Around 10–15% of all ischaemic strokes are linked to carotid stenosis. Because stroke is one of the leading causes of disability and death, recognising and managing carotid stenosis is important.
Causes and risk factors
The most common cause is atherosclerosis, but several factors increase the risk of developing it:
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
- Obesity and lack of exercise
- Older age
- A history of cardiovascular disease
These risks often combine, making lifestyle changes and medical treatment essential in slowing or preventing disease progression.
Symptoms
Many people with carotid artery stenosis do not have symptoms until the narrowing becomes severe or causes an event. Possible symptoms include:
- A transient ischaemic attack (TIA) with sudden weakness, speech problems or numbness lasting less than 24 hours
- Stroke with more permanent neurological symptoms
- Temporary loss of vision in one eye, described as a dark curtain coming across the vision (amaurosis fugax)
If stenosis has not yet caused symptoms, it is often discovered incidentally, for example when a doctor hears a bruit in the neck.
How carotid stenosis is diagnosed
The first-line test is duplex ultrasound, a painless scan that uses sound waves to measure blood flow and detect narrowing. If intervention is considered, further imaging such as CT angiography or MR angiography can give more precise information about the artery’s structure and the location of the plaque.
Treatment approaches
The treatment of carotid artery stenosis has two main aims: to reduce the risk of stroke and to manage risk factors for atherosclerosis.
Medical treatment is important for everyone with carotid stenosis. This usually involves antiplatelet therapy (such as aspirin), cholesterol-lowering medication, strict blood pressure and diabetes control, and lifestyle measures such as stopping smoking and maintaining a healthy weight.
When the narrowing is severe (often 70% or more) and the patient has already had symptoms such as a TIA or stroke, a procedure to reopen the artery can greatly reduce the chance of another stroke.
Carotid revascularisation
Revascularisation means restoring blood flow by opening the blocked artery. Two main procedures are used:
- Carotid endarterectomy, where the surgeon makes an incision in the neck, opens the artery and physically removes the plaque.
- Carotid stenting, where a stent (a small metal mesh tube) is placed inside the artery to hold it open and keep blood flowing.
Both procedures carry risks, and the choice depends on factors such as the patient’s overall health, anatomy of the blockage and local expertise.
Carotid stenting in detail
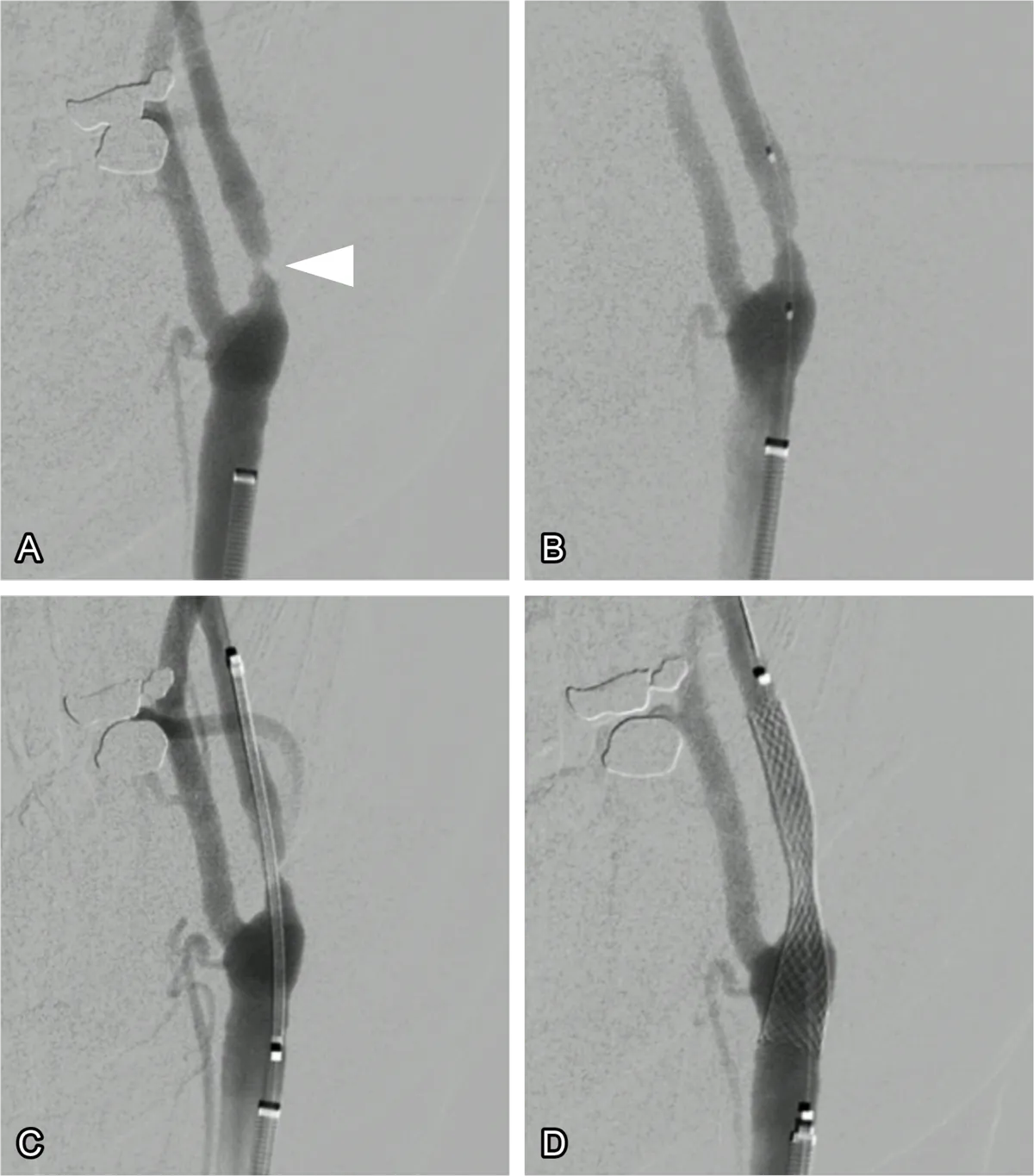
Carotid stenting is a minimally invasive treatment designed to reduce the risk of stroke in people with significant carotid stenosis. Instead of making a large incision in the neck, doctors use thin tubes (catheters) to reach the carotid artery, usually through an artery in the leg (femoral access), sometimes the arm (radial access), or directly through the neck just above the collarbone (a technique called TCAR, or transcarotid artery revascularisation).
A small balloon may be used to widen the artery before placing the stent. The stent is then positioned across the narrowed segment (fig. 1). Once expanded, it stays in place permanently, acting as a scaffold that keeps the artery open. Modern procedures also use protection devices or flow-reversal systems to reduce the chance of plaque debris travelling into the brain during the procedure.
Benefits and outcomes of stenting
Carotid stenting offers several advantages compared with open surgery: it is less invasive, involves smaller or no neck incisions, and usually has a shorter recovery time. For most patients, blood flow improves immediately, lowering the risk of stroke.
Studies show that stenting and endarterectomy have similar long-term effectiveness, though stenting may carry a slightly higher risk of minor stroke, while endarterectomy carries a higher risk of nerve injury. Both procedures are generally durable, with more than 95% of patients maintaining good artery function long-term.
Risks of stenting
Like any procedure, carotid stenting has potential risks, including stroke, bleeding at the puncture site, damage to the artery, low or high blood pressure during the procedure, or, rarely, death. The risks vary depending on the severity of the disease and the patient’s overall health.
Life after stenting
Carotid stenting does not cure atherosclerosis. Patients must continue with risk factor control and medication to prevent further plaque build-up, both in the treated artery and elsewhere in the circulation. Regular follow-up imaging of the carotid arteries is recommended.
Most patients return to normal activities within a week. Long-term success depends on maintaining healthy lifestyle habits, taking prescribed medicines, and keeping blood pressure, cholesterol and diabetes well controlled.
Stroke