Treatment of DAVF
Treatment approaches for DAVFs, including endovascular embolisation, surgical excision, and risk considerations.
The goals of treating a dural arteriovenous fistula are twofold: to relieve symptoms and to reduce the risk of serious bleeding around the brain in the future. The mainstay of treatment is endovascular therapy, in which a catheter is guided through the blood vessels to the site of the fistula. Special materials such as coils, glue or other embolic agents are then used to block the abnormal connection between arteries and veins, restoring more normal blood flow.
How can endovascular treatment help?
“Endovascular” means that access to the brain or surroundings is achieved by threading a very fine tube through your arteries. Embolisation is a way of blocking abnormal blood vessels and is usually carried out to prevent the DAVF from bleeding. This is done by injecting a special glue-like liquid into the DAVF to cut off the blood vessels supplying the fistula.
What happens during the embolisation procedure?
Dural arteriovenous fistula (DAVF) embolisation is carried out under general anaesthesia in the angiography suite and typically takes between one and three hours. A multidisciplinary team of radiologists, radiographers, anaesthetists and nurses monitors the patient closely throughout.
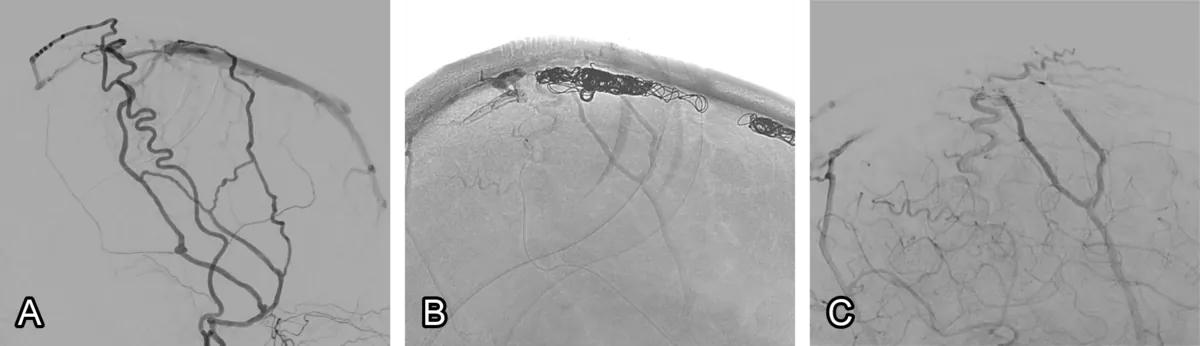
The procedure begins with the insertion of a thin, flexible plastic tube (catheter) into either the femoral artery in the groin or an artery in the wrist. The catheter is advanced through the aorta into the cerebral arteries of the neck and brain. Once the most accessible feeding vessel is identified, additional catheters, including a microcatheter, are introduced to reach the point of the fistulous connection (fig. 1). Embolic material, often glue-like in consistency, is then injected to occlude the DAVF. In some cases, small platinum coils are deployed in addition. The embolic material forms an artificial clot, preventing further abnormal blood flow into the fistula. X-rays are obtained throughout to confirm successful obliteration.
At the end of the procedure, the catheters are removed and the puncture site in the groin or wrist is sealed with a collagen plug or controlled manually to prevent bleeding. The procedure usually takes 2–3 hours.
Will it hurt?
The procedure is performed under general anaesthesia, so no pain is experienced during the intervention. Some discomfort may occur afterwards at the wrist or groin access site, but this is usually mild and resolves with simple analgesics.
What are the risks of DAVF embolisation?
All medical procedures carry risks, and for dural arteriovenous fistula (DAVF) embolisation these depend on the size, position and configuration of the vessels.
Contrast dye risks – The iodine-based dye used to show the blood vessels on X-ray can occasionally cause an allergic reaction (ranging from mild rash to severe reaction needing urgent treatment) and can sometimes affect kidney function, especially in people with pre-existing kidney problems. A blood test may be done beforehand to check kidney function.
Risks of the general anaesthetic – As with any general anaesthetic, there are some risks such as sickness or sore throat, and very rarely more serious complications.
Stroke – The main risk of the procedure is stroke, which occurs in about 5 in every 100 people. A stroke can cause weakness, problems with speech, or changes in vision. These effects can sometimes be temporary but may also be permanent.
Severe brain injury or death – There is a very rare risk of a severe brain injury that can result in death, estimated at about 1 in every 100 patients.
Radiation exposure – The X-rays used carry a very small long-term risk of developing cancer, and very occasionally can cause temporary hair loss or skin redness around the treated area.
Bruising at the access site – The procedure is usually done through a small tube in the wrist or groin. Bruising in this area is common and generally minor, though rarely the bruise can become large and may need further treatment, including surgery.
Are there any alternatives?
Surgical excision is an alternative treatment in which a craniotomy (skull incision) is performed to directly access the DAVF. The feeding arteries and draining veins are then clipped and disconnected. This is a well-established but more invasive treatment that can provide lasting protection against rupture or haemorrhage. Surgical excision also carries its own specific risks.
What happens after the embolisation?
On arrival to the ward, a period of bed rest is required for recovery. During this time, the nursing staff carry out regular checks, including inspection of the catheter entry site in the groin to ensure there is no bleeding. If bleeding occurs, the period of rest is extended. Some bruising and soreness around the groin is common, but most patients experience little or no after effects. Most commonly patients go home the day after treatment.
DAVF